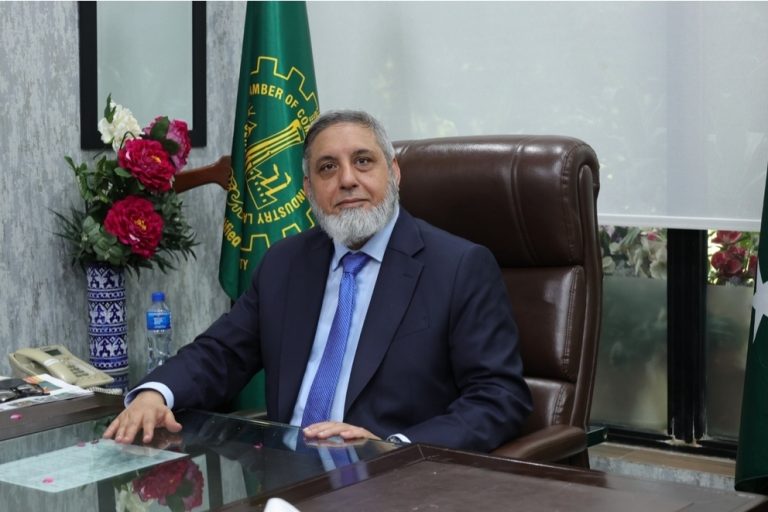
Dr Alamdar Hussain Malik
Advisor, Veterinary Sciences
University of Veterinary and Animal Sciences, Swat Former Secretary / Registrar, Pakistan Veterinary Medical Council
The interconnection between human, animal, and environmental health is one of the greatest challenges of our time. Approximately 60% of known infections and more than 75% of emerging infectious diseases originate from animals, including livestock, wildlife, and shared ecosystems. The concept of One Health was first introduced in 2004 through collaboration between the World Health Organization (WHO), FAO, and other international bodies, and after 2010, various countries began implementing it practically. The purpose of this approach is to integrate human and animal health to reduce the risks of zoonotic diseases and antimicrobial resistance (AMR). In Pakistan, millions of rural families depend on livestock for livelihood, nutrition, and income, which increases the risk of disease transmission between humans and animals. Frequent close and often unhealthy contact, inadequate veterinary services, weak surveillance, and improper use of medicines have amplified these risks. The consequences are severe: livestock losses affect rural economies, zoonotic diseases impact human health, pregnant women may face miscarriages and complications, and emerging pathogens can pose systemic threats. Increasing AMR further complicates the crisis, turning otherwise treatable diseases into potentially fatal ones. This makes the immediate implementation of a structured One Health strategy in Pakistan imperative.
The ineffective coordination between human and animal health sectors has accelerated these risks. Unregulated use of medicines, poor nutrition, contaminated water, unregulated livestock markets, and increased human-animal interaction have accelerated disease spread. In most rural areas, humans and animals live in close proximity, basic hygiene and vaccination services are limited, and systems for timely disease detection and treatment are almost nonexistent. Millions of people rely on their animals’ health, and if animals fall ill, both human health and rural economies are impacted.

Some measures have been taken so far. Pakistan has developed a National Action Plan for AMR, and some provincial veterinary and health departments have conducted workshops and training sessions. International organizations and donor agencies, such as WHO and FAO, provide funding and run training programs. However, the real problem is that these programs mostly remain confined to high-level meetings, reports, and seminars, while real stakeholders—local communities and field veterinarians—have limited access. Funds and resources are often used only for reporting and international partnerships, with minimal impact on the ground, which increases public health risks.
Most responsible individuals belong to the bureaucracy, possess limited practical and technical knowledge, and are frequently transferred to other positions. This undermines sustained leadership and effective implementation. Only trained, practical, and technical experts should be involved in One Health implementation to ensure effective actions and risk reduction.
It is also concerning that the importance of One Health is not widely known even among graduates and postgraduates. Universities, the Federal Higher Education Commission (HEC), and Provincial HECs are responsible for including One Health in curricula, providing research and training opportunities, and equipping the new generation with practical knowledge. Without this, implementation is affected, and future generations will not be prepared to face these challenges.
Specifically, One Health must be made an integral part of the Doctor of Veterinary Medicine (DVM) curriculum. Veterinary students should be introduced from the beginning to zoonotic diseases, the relationship between human and animal health, biosecurity, vaccination, and principles of AMR. The curriculum should include One Health modules, practical training, internships, and joint sessions with human health institutions so that DVM graduates understand real-world disease risks and can take practical action. Without incorporating One Health into the DVM curriculum, the training of the new generation remains inadequate, and the implementation of One Health in Pakistan will remain delayed and ineffective.
The federal government plays a fundamental and decisive role in this system. A National One Health Secretariat must be established to provide leadership, coordinate provincial implementation, ensure proper allocation of funds, and strengthen partnerships with international organizations. The federal government must ensure that provincial departments, universities, HECs, and donor agencies are working on the ground and not limited to seminars and reports. Without the federal government, integrated surveillance, data quality, timely responses, and practical implementation are impossible. Furthermore, it must ensure that the majority of funds are spent on real stakeholders rather than high-level meetings and five-star hotel seminars. This step is crucial to reduce public health risks and make One Health effective.
Livestock, veterinary, and human health stakeholders must receive practical training to identify diseases early, carry out vaccination, maintain biosecurity, and ensure proper use of medicines. They must also understand that One Health integrates human, animal, and environmental health, reduces zoonotic disease and AMR risks, and safeguards food security and the economy. Without practical training, regulations and instructions are insufficient, and risks increase in rural areas where basic knowledge and facilities are lacking. Donor agencies, which often hold seminars in five-star hotels, should use their funds for practical, on-farm training.
If immediate and coordinated actions are not taken, human lives, food security, livelihoods, the economy, and national resilience against epidemics will be at risk. Every epidemic, whether in humans or animals, signals a national threat. Pakistan’s citizens cannot afford delays. One Health must be given immediate, practical, and unconditional priority; otherwise, the risks of diseases, AMR, and weak surveillance will prove catastrophic for public health, food security, and the economy.